Researchers at the University of British Columbia have created an artificial intelligence that can identify a subset of endometrial cancer patients that are at higher risk of recurrence or death from disease.
Endometrial cancer is the most common gynecological cancer globally and the fourth-most common cancer for people assigned female at birth, said Dr. Jessica McAlpine, one of the lead researchers. McAlpine is a professor and the Dr. Chew Wei Chair in gynaecologic oncology at UBC. She is also a surgeon-scientist at Vancouver General Hospital and BC Cancer.
Endometrial cancer cases are on the rise, and in a decade or so endometrial cancers will likely be the second most common cancer after breast cancer, she added.
Her research is working to help improve patient care by flagging which patients need treatment to be scaled up and which ones can have treatment scaled down.
“We want to be catching the baddies and sparing those who don’t need chemo and radiation,” said McAlpine said.
Her team’s research was recently published in the journal Nature Communications.
There are a number of reasons why the team is excited about this discovery.
To start, the AI has been able to flag higher-risk cancers, which is something oncologists are not able to do with existing diagnostic tools, McAlpine said.
Pathology and molecular diagnostics can sort endometrial cancers into four subtypes, with helps doctors understand the risk of each cancer, McAlpine said.
However, the largest of these subtypes — which makes up roughly half of all cases — can have widely varied patient outcomes. The AI is helping doctors understand which patients in this subtype of cancer are at the highest risk.
The new tech could improve patients’ lives
The AI is still in its research phase and has been learning by analyzing over 2,300 images of endometrial cancer from a research library. Next, McAlpine says the team wants to analyze images from 100 patients currently being diagnosed with endometrial cancer to see if the AI can predict what patients are more likely to experience disease recurrence.
If everything works, after a year and a half, the team may be looking to scale up the AI for use across Canada or even a global audience — but that will depend on regulatory approval, McAlpine said.
The AI has the potential to help improve patient care because doctors will be able to identify what patients need more comprehensive care and which ones would not require additional treatment after surgery, she said.
To move a patient and their family to Vancouver or Victoria for specialized cancer care can have an enormous financial, social and structural impact on patients, McAlpine said.
It’s expensive to drive or fly down to the south coast of B.C. from elsewhere in the province, to find housing and for family to take time off work.
It can remove a matriarch who holds a supporting role in her community. It can even be dangerous to have people drive on winter roads across the province.
If successful, the AI could identify those who need specialized surgery, radiation and chemotherapy. And those who need more straightforward surgeries can likely have those surgeries done in a hospital close to their home.
It would help patients stay in their community whenever possible.
Into the lab
Now that the AI model has been built, it’ll be relatively easy to add computing power to scale up to serve the province, Canada or a larger audience, says Ali Bashashati, also a lead researcher in the study.
Bashashati is an assistant professor of biomedical engineering and pathology and laboratory medicine at UBC and director of AI research at the Ovarian Cancer Research Program at BC Cancer.
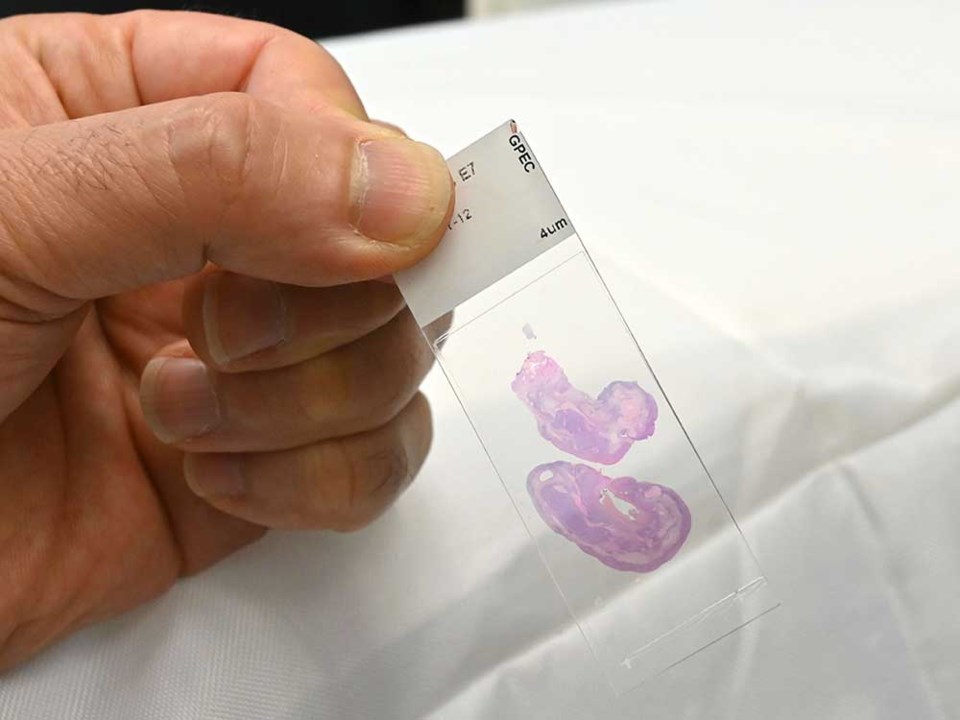
The AI analyzes images from hematoxylin and eosin-stained slides, or thinly-sliced tissue samples that scientists look at under microscopes.
This is medical technology that has been widely used for the last 150 years, Bashashati said, so most labs will be able to produce a sample to be analyzed.
From there, the sample will need to be scanned to make an extremely detailed digital copy for the AI to analyze. If the necessary scanner isn’t available, the slide can be mailed to a lab that has one — no biohazard declaration necessary, he said.
To help explain further, Bashashati pulls up an image of a scanned slide on his computer screen. It looks a bit like a pink continent against a white ocean, complete with frilly coastlines and jagged mountain ranges.
Although the tissue sample on the slide is the size of a fingernail, the digital image fills the screen.
Then he zooms in, and zooms in again and again until a cluster of red blood cells fills the screen.
To get this image, researchers will slice a biopsied tumour to around four microns thick — 16 times thinner than a human hair — lay it on a thin glass rectangle called a slide, and then stain it with hematoxylin and eosin, which gives the cells a pink or blue colour.
The slide can be placed under a microscope to be examined by a pathologist.
Bashashti’s team has scanned the slide and created a digital image roughly 100,000 pixels tall by 100,000 pixels wide. (For comparison, a picture run on The Tyee’s website will generally be 1,000 pixels wide).
Each image can contain three-to four gigabytes of data.
It’s a bit like taking a picture of the Lower Mainland from an airplane but taking such a detailed picture that you could zoom in and count the sugar ants scattered across the city.
A pathologist will, to stick with the metaphor for a minute, be the one looking for the sugar ants.
For many cancers, a pathologist can accurately identify what they’re looking at and what it means for the patient, Bashashati said.
But for this one subtype of endometrial cancer, a pathologist wasn’t able to see what cases would be higher risk. And molecular diagnostics weren’t able to identify it, either.
Molecular diagnostics look for the presence or absence of proteins in cells and can examine DNA to look for specific mutations, McAlpine said.
What remains to be understood
If approved for regular use, the AI would be used as a third level of testing that could be run after pathology and molecular diagnostics, she added. It would not replace these diagnostics.
And there are still areas of research that are yet to be understood, including how ethnicity impacts health outcomes.
McAlpine says many places in Canada don’t collect race-based data and BC Cancer only started collecting race-based data for patients getting surgery in Vancouver in January 2023. She didn’t yet know if there was disparity in health outcomes for Indigenous or Black patients in Canada.
In Seattle, Washington, the Fred Hutch Cancer Center said on their website that while Black and white patients are equally as likely to get endometrial cancer, Black patients are nearly twice as likely to die from it.
This is due to several factors, according to the Center. Black patients are often diagnosed at later stages of the disease. Black patients have a 30 per cent delay in diagnosis compared to white patients, and they are less likely to receive surgery, according to research by Dr. Kemi Doll, a gynecologic oncologist at the Fred Hutch Cancer Centre.
The Tyee reached out to Doll to ask what the impacts of using AI as part of a diagnostic tool could be, but did not hear back by press time.
Back in Vancouver, McAlpine notes the urgency with which researchers are working to improve diagnostic technology for endometrial cancer.
Endometrial cancer and liver cancer are the only cancers in Canada where the rate patients die from the disease is slowly rising, she said, adding that liver cancer is far more rare than endometrial cancer.
McAlpine said the rise in cases is partially attributed to people living longer, bodies being overall heavier and fewer people getting hysterectomies than they used to. A hysterectomy is the complete removal of the uterus.
Previously doctors would recommend a hysterectomy if a patient had abnormal vaginal bleeding, similar to how they used to recommend surgery to remove a patient’s tonsils or appendix if there was an infection, McAlpine said.
However, longer lives, heavier bodies and fewer hysterectomies do not fully explain the rise in cases, she added.
“There’s still a lot that isn’t fully understood.”